Education
Eye Conditions
Eye Diseases
Normal Vision
Normal Vision
For perfect clear vision, what we see (an image) needs to be focused onto the retina, just like a camera has to be focused properly in order to take a clear picture.
If the image is not focused exactly on the retina, then the image will be blurred, just like an out-of-focus photograph. In this case, the person is said to have a refractive error.
Refractive errors occur when there is a mismatch between the length of the eye, and its optical power. These mismatches usually originate during childhood, when the eyes are growing. The exact causes of refractive errors are still being studied, but it is known that both hereditary and environmental influences can affect their development.
Most people have some refractive error, but in most cases the error is small, and does not cause any problems. Above the age of 40, it is normal for the near reading vision to become slightly blurred. This is due to presbyopia.
Myopia
Myopia | Short Sightedness
What is Myopia?
Myopia is what most people call short-sightedness. Short-sighted people do not see distant objects clearly. The eye’s lens and cornea normally focus light into an image on the retina. In a myopic eye the light is focused in front of the retina and so the image is blurred.
Does a short-sighted person see close objects more clearly than a person with normal vision?
No. Short-sighted people see close objects equally as well or sometimes slightly worse. When their myopia is corrected, they see objects equally as well.
How can I tell if I am shortsighted?
Shortsighted people have difficulty in seeing distant objects clearly. They find it hard to read road signs and scoreboards. Recognising people in the distance and playing ball games also may be a problem for many short-sighted people. Often a person will not realise that they cannot see clearly but an eye examination by an optometrist will reveal the problem.
How can I tell if my child is shortsighted?
A complete eye test is the only sure way of determining whether your child’s vision is normal. Some clues to myopia in a child are:
- Squinting eyes to see distant objects.
- Difficulty in reading the blackboard at school.
- Poor posture while reading.
- Lack of interest in playing outdoor games.
What causes Myopia?
Myopia is caused by a mismatch between the power of the optical components of the eye and the length of the eye (the ‘axial length’). Either the power is too high, or the length is too long, or both. Usually the cornea (the front surface of the eye) is curved more steeply than average, increasing its optical power. The exact causes of the mismatch between power and axial length are unknown. There is some genetic influence (if your parents are short-sighted, you have a greater chance of being short-sighted yourself), and there is some evidence for environmental factors, such as excessive amounts of near work, having some influence.
Can Myopia be cured?
No, but properly prescribed spectacles or contact lenses will enable the person to see clearly. The lenses diverge incoming light rays, so that they will be properly focused on the retina. There are also a number of techniques available for re-shaping the cornea (the front surface of the eye), in order to reduce its power and thus correct the myopia. One technique (known as orthokeratology or ‘Ortho-K’) uses rigid contact lenses to change the shape of the cornea while you sleep so that you can be free of contact lenses and glasses during the day. Other surgical techniques use lasers or implants to change the power of the front of the eye.
Can Myopia be prevented?
There is no certain prevention for myopia. However, in some cases, treatment can be prescribed to stop or slow its progression.
Recent research indicates that lowered rates of myopia are linked with outdoor activity of 10-14 hours per week. One thought as to why outdoor activity at a young age can reduce myopia progression is that sunlight stimulates retinal dopamine. This in turn inhibits eye growth and therefore also myopia.
How common is Myopia?
It is a very common condition. With approximately 15% of the population being short-sighted. Usually myopia starts to develop in teenage years and may get worse in early adulthood.
Can Myopia cause other problems?
High levels of myopia can cause other, more serious problems. People with high levels of myopia often have very large, elongated eyes, and their retinas may be stretched and thinner than normal. This increases the risk of the retina developing holes and tears and the risk of retinal detachments. If you are myopic you should have regular eye examinations, and talk to your optometrist about the potential for problems.
Astigmatism
Astigmatism
What is Astigmatism?
Astigmatism is a focusing error that causes asymmetric blur. Some directions in an image are more out of focus than others. This can be contrasted with short-sightedness (Myopia) where all directions are uniformly blurred.
What does it look like?
Astigmatism causes different amounts of blur in different directions. This causes images to appear distorted, or sometimes even double. Certain letters may be more difficult to read than others, depending on the orientation of the lines within them.
One type of chart used to detect Astigmatism uses a series of lines arranged in a fan shape – if you have Astigmatism, some lines will appear clearer than others.
What causes Astigmatism?
Most Astigmatism is caused by the irregular shape of the front surface of the eye (the cornea). It can also be caused by slight tilting of the lens inside the eye. It may be an inherited characteristic or a normal variation accompanying growth.
Can you describe the shape?
A magnifying glass focuses the sun to a point image because its two surfaces are spherical, each like the surface of a basketball. Now imagine a transparent surface shaped like the side of an Australian Rules or rugby football. It has two different curvatures. These result in light focusing at two different locations. The image does not focus to a point and so is blurred.
How does Astigmatism affect me?
Objects at all distances are indistinct or blurred and the eye cannot focus. Even slight degrees of astigmatism may encourage headaches, fatigue and reduce concentration. The eyes may try, without success, to correct the blur. There is also a tendency to squint the eyes to try to see better, producing discomfort in the muscles of the eyelid and face.
How is Astigmatism corrected?
Spectacles and contact lenses (hard and soft) can correct Astigmatism. Sometimes correction of Astigmatism can cause a change in the apparent size and shape of objects and may affect judgment of distance. A patient may feel taller or shorter or see objects appearing to slope and curve.
In most cases, adjustment to these side effects takes only a week or so. Astigmatism correction may involve a compromise between optimal clarity and visual discomfort.
How is Astigmatism detected?
Some people notice blur themselves. Only a proper eye examination will determine for certain if you have Astigmatism. Astigmatism is not an eye disease and any changes are generally gradual and not necessarily for the worse. Most people have at least very slight Astigmatism.
Colour Vision Deficiency
Colour Vision Deficiency
What is Colour Vision Deficiency?
Colour vision defects are almost always inherited, although some forms can be an acquired condition as a result of some diseases or injuries.
The abnormality is sex linked, recessive, and carried on the X chromosomes. Males have one X chromosome and females have two. In relation to colour defects, this means that any males that have a defect on their one X chromosome will exhibit a colour vision defect, while females must carry the same type of colour vision defect on both their X chromosomes to be colour vision deficient. If females have it only on one X chromosome they will carry the condition but still have normal colour vision themselves.
In the general population, about 8% of males and 0.5% of females have colour vision deficiencies. Almost all colour deficient people do see a large range of colours but they will have difficulty identifying particular colours. The most common defects lead to confusing certain shades of red and green for example.
As children, few of these people will be aware that they have a colour vision deficiency but the detection of these problems is important, especially when career choices are affected.
See Below for an example of an Ishihara Colour Vision Examination Plate:
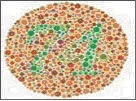
A colour vision assessment can be carried out by one of our qualified optometrists.
Presbyopia
Presbyopia
What is Presbyopia?
Presbyopia is a common condition that makes vision difficult at a normal reading distance. It is not a disease.
How will Presbyopia affect my vision?

Initially, close tasks such as reading and sewing become difficult, particularly under poor lighting conditions. Later, even tasks further away such as laptop or computer use may become difficult. For example, initially you may find that you are holding your newspaper further away from your eyes to make the print clearer. Presbyopia does not affect distance vision. You may also have difficulty concentrating when reading, or you may find periods of close work result in sore eyes, headaches or tiredness.
What causes Presbyopia?
It is important to understand how your eyes change their focus for viewing close objects. Normally they are focused for distance vision. Inside the eye there is a lens about the size of a pea. To focus on close objects, a special muscle in the eye changes the shape of the lens. This process is called accommodation.
With age the lens loses its flexibility and is less able to change its shape. This is a completely normal ageing change, just like stiffening joints or greying hair. The loss in lens flexibility is the reason that close focusing becomes more difficult.
Who is likely to become presbyopic?
Everyone experiences the ageing process that causes presbyopia. The condition cannot be prevented.
Does Presbyopia come on quickly?
No. Presbyopia is usually first noticed around the age of 40 to 45 years. Although difficulties with close work may seem to come on suddenly, the ageing process that causes presbyopia is gradual and has been going on since childhood. Between the ages of 45 and 65 the amount of presbyopia increases, making near work more difficult. From 65 years onwards, there are unlikely to be any further significant changes to vision due to presbyopia.
How is Presbyopia treated?
Presbyopia is corrected with either spectacles or contact lenses with a prescription designed especially for close distances. It is important that the prescription is calculated for the distance at which you do your close tasks.
Discussion with your optometrist will help to determine the best way of preparing your prescription. The correction for presbyopia will make near objects clear but distant objects blurry. This means that if you have a pair of spectacles just for reading you will not be able to watch television while wearing them.
Having different prescriptions for distance and reading can be a nuisance, especially if you have to change spectacles all the time. One way around the problem is the use of a multifocal. These are special lenses that have a prescription for distance vision in the top half of the lens and a gradual progression in power to the reading prescription in the lower half.
Does Presbyopia mean that my eyes are deteriorating?
No. Although your close focusing system is not functioning as well as it used to, once Presbyopia has been corrected with spectacles you will be able to see close things as well as you always did. Presbyopia does not represent a threat to your eyes’ health.
When should I have my prescription for Presbyopia renewed?
Between the ages of 45 and 65 your prescription is likely to change significantly. Its recommended to have your eyes examined every two years to review your prescription and your general eye health. If you experience vision problems within two or three years of your previous examination you should make a review appointment with your optometrist. Your optometrist will advise you of the most appropriate period between consultations.
Will wearing spectacles weaken my eyes?
No. Presbyopia will continue regardless of whether spectacles are worn. Wearing spectacles will not accelerate or slow the development of Presbyopia.
Cataracts
Cataracts

What are Cataracts?
Cataracts are cloudy areas that form in the lens of the eye. The lens is normally clear. Poor vision results because the cloudiness interferes with light entering the eye. The opacities in the lens scatter the light, causing hazy vision, in the same way that a dirty window scatters light and is more difficult to see through.
Are Cataracts a kind of growth?
No. Cataracts are due to a change in the lens material, they are not an extra part growing within the eye. Cataracts can become worse as more of the previously normal lens material changes.
What causes Cataracts?
Most Cataracts are a result of ageing and long-term exposure to ultraviolet light. Some are caused by injury and certain diseases and in rare cases by exposure to toxic materials and radiation. Occasionally Cataracts are present at birth, this can be due to the baby’s mother having had rubella during the pregnancy, or be a genetic defects.
Do Cataracts get worse?
Yes. The clouded areas become larger and denser and cause sight to become worse. The time taken for this to happen varies from a few months to many years.
Do Cataracts affect both eyes?
Usually Cataracts affect both eyes but often develop at different rates in each eye.
How common are Cataracts?
People older than 65 years often have signs of Cataracts and should have their eyes examined regularly. The severity of cataract varies considerably between individuals of the same age.
Can Cataracts cause blindness?
If untreated, Cataracts can cause blindness. Blindness can be prevented by detecting the Cataracts early and, if necessary, by having them removed surgically. Your optometrist will refer you to an eye specialist if they consider that you need surgical treatment for your Cataracts.
How well will I see if my lens is removed?
In most cases very well. Most patients have an intra-ocular lens (IOL) inserted at the time of surgery, with excellent results. This is a clear plastic lens that replaces your own cloudy one. Patients may still need to wear spectacles or contact lenses after surgery.
What are the signs of Cataracts?
Usually the development of Cataracts is gradual with a painless worsening of sight. Other symptoms include blurred or hazy vision, spots before the eyes, double vision and a marked increase in sensitivity to glare.
How can I be sure I don’t have Cataracts?
An examination by your optometrist will reveal any changes that have occurred in the lens of the eye. Optometrists have special equipment that enables them to see changes in the lens that may lead to Cataracts several years before any symptoms appear.
Can Cataracts be prevented?
There is no proven method of preventing Cataracts. Long-term exposure to ultraviolet light is thought to induce Cataracts, so a brimmed hat and Australian approved sunglasses should be worn in sunlight.
When should I have a Cataract operation?
This varies with each patient. Usually cataract surgery is performed when the patient’s vision interferes with their daily life. Your optometrist will assist you in making this decision.
Is Cataract removal a major operation?
Cataract surgery is now a relatively minor procedure. Often it is performed under a local anaesthetic. Depending on the patient, the surgery may be performed on an out-patient basis. This means that the patient attends a hospital or clinic for the surgery and is able to go home the same day. The surgery is performed by an ophthalmologist, a medical doctor who specialises in eye surgery. Your optometrist will refer you to an ophthalmologist when necessary.
Conjunctivitis
Conjunctivitis

What is conjunctivitis?
Conjunctivitis is an inflammation of the conjunctiva, the thin, transparent layer covering the surface of the inner eyelid and a portion of the front of the eye. This condition appears in many forms and affects people of all ages.
What causes conjunctivitis?
The three main types of conjunctivitis are infectious, allergic and chemical. The infectious form, commonly known as “pink eye” is caused by a contagious virus or bacteria. Your body’s allergies to pollen, cosmetics, animals or fabrics can often bring on allergic conjunctivitis. And, irritants like air pollution, noxious fumes and chlorine in swimming pools may produce the chemical form.
What are the signs/symptoms of conjunctivitis?
Common signs/symptoms of conjunctivitis are red eyes, inflamed inner lids, watery eyes, blurred vision and a sandy or scratchy feeling in the eyes. With the infectious form, there may be a puss-like or watery discharge around the eyelids. Since infectious conjunctivitis is contagious, measures should be taken to prevent spreading this condition. To avoid giving infectious conjunctivitis to others, keep your hands away from your eyes; thoroughly wash your hands before and after applying eye medication; do not share towels, flannels, cosmetics or eyedrops with others and seek treatment promptly. Small children, who may forget these precautions, should be kept away from school and the swimming pool until the condition is cured.
Diabetes
Diabetes
Diabetes and Diabetic Retinopathy
What is Diabetic Retinopathy?
Patients with diabetes are more likely to develop eye problems such as cataracts and glaucoma, but the disease’s affect on the retina is the main threat to vision. Most patients develop diabetic changes in the retina after approximately 15 years of the disease. The effect of diabetes on the retina is called diabetic retinopathy.
In this condition the small blood vessels in the retina become weakened and leak, forming small hemorrhages. The leaking of the vessels often leads to swelling in the retina and decreased vision. If untreated circulation problems can occur in these vessels and the retina becomes deprived of oxygen. This leads to death of the cells in the retina and a permanent loss of vision.
If you are diabetic the National Health and Medical Research Council recommends yearly dilated eye examinations so that related eye problems can be detected and treated as early as possible. At our practice we perform detailed dilated fundus examinations on all diabetics. We communicate with your general practitioner (GP) and also ophthalmologists (Eye specialists) to give you the best possible care.
There are two main types of this condition: background retinopathy and proliferative retinopathy. The risk of developing retinopathy increases with the length of time you have had diabetes. The risk is also increased by poor control of blood sugar levels and blood pressure levels.
Background Retinopathy
This is the more mild form of diabetic retinopathy. This may involve hemorrhages and leaking blood vessels. More serious complications include swelling of the retina which may cause vision loss. This stage of retinopathy indicates that the blood sugar levels are not within appropriate levels.
Proliferative Retinopathy
This condition is more serious and requires early treatment to prevent serious vision loss. Your optometrist can recognise signs that this condition might develop, or detect it in its early stages. Once proliferative retinopathy has been diagnosed, your optometrist will refer you to an eye surgeon for further appraisal and probable laser treatment. Treatment of this condition has a better chance of success if it is applied very early.
Managing Diabetic Retinopathy
The time at which diabetic retinopathy begins is not predictable. Some people can have diabetic retinopathy upon being diagnosed with diabetes and others will have no signs of retinopathy even 15 years after being diagnosed with diabetes. The best management is to have regular eye examinations so that changes can be detected and treated early. It is advisable for all people with diabetes to have yearly eye examinations. People who have been diagnosed as having retinopathy should have eye examinations more frequently than once a year.
Diabetes and other vision conditions:
Double vision
This is a distressing but rare complication of diabetes. The condition is usually temporary but it may last for a few months. An optometrist can help treat it while it has effect. Diabetes is not the only cause of double vision.
Glaucoma
The eye disease Glaucoma is slightly more common in diabetic people than in the general community. Glaucoma is a condition in which the nerve cells that transmit information from the eye to the brain become damaged, often caused by pressure due to a build-up of fluid in the eye. If untreated, Glaucoma can cause blindness.
Cataract
Cataracts are more likely to occur in diabetic people at an earlier age than in non-diabetic people. A cataract is a cloudiness that can form in the lens inside the eye. If present, Glaucoma and cataract will be readily detected at your regular eye examination when your optometrist will advise the best management strategy for the condition.
Dry Eye
Dry Eye
What is “Dry Eye?”
The tears your eyes normally produce are necessary for overall eye health and clear vision. Dry eye occurs when your eyes do not produce enough tears or produce tears which do not have the proper chemical composition.
What causes Dry Eye?
Dry eye symptoms can result from the normal ageing process, exposure to environmental conditions, problems with normal blinking or from medications such as antihistamines, oral contraceptives or antidepressants. Dry eye can also be symptomatic of general health problems, other diseases or can result from chemical or thermal burns to the eye.
What are the Signs/Symptoms of Dry Eye?
The most common signs/symptoms include burning, stinging, itchy, scratchy, gritty and uncomfortable eyes. You may experience increased dry eye symptoms on waking. Some people experience watering eyes. This is a natural reflex to comfort a dry eye.
How is Dry Eye diagnosed?
During the examination, your optometrist will ask you questions about your eye comfort, general health, your use of medications and your home and work environments to determine any factors which may be causing dry eye symptoms. This information will help us to decide whether to perform dry eye tests. These tests allow your optometrist to evaluate the quality, the amount and the distribution of tears to detect signs of dry eyes.
Can Dry Eye be cured?
Dry eye cannot be cured, but your eyes’ sensitivity can be lessened and measures taken so your eyes remain healthy. The most frequent treatment is the use of artificial tears or tear substitutes. For more severe dry eye, ointment can be used, especially at bedtime. Other treatments involve warm eyelid compresses and massage. In some cases, small plugs may be inserted in the corner of the eyelids to slow drainage and loss of tears.
Will Dry Eye harm my eyes?
If dry eye is untreated, it can harm your eyes. Excessive dry eye can damage tissue and possibly scar the cornea of your eye, impairing vision. Dry eye can make contact lens wear more difficult due to increased irritation and a greater chance of eye infection. To keep dry eye symptoms in check, you and your optometrist need to work together.
If you have increased dryness or redness that is not relieved by the prescribed treatment, let us know as soon as possible.
If you continue to have discomfort, the drops may be used more frequently or as needed. You should return for follow-up care as recommended.
Glaucoma
Glaucoma
What is Glaucoma?

Glaucoma is a condition in which the nerve cells that transmit information from the eye to the brain become damaged. This prevents visual information from getting from the retina in the eye to the brain. Glaucoma is often linked with a build up of pressure in the eye. The eye is filled with fluid that is constantly being replaced. If excessive amounts of fluid are produced, or if it cannot drain away properly, the pressure inside the eye can increase. In some forms of Glaucoma, the pressure inside the eye can become extremely high, but in other forms the pressure may remain normal.
What causes Glaucoma?
The exact causes of Glaucoma are not known. In some cases the drainage network of the eye may not be formed properly, or may become blocked by natural materials or due to injury; in other cases there is no clear cause.
Is the damage that occurs in Glaucoma serious?
If untreated, Glaucoma can cause blindness. As the nerve cells are progressively damaged, the ability to see objects in different parts of the visual field and your peripheral vision is lost. The damage to the nerve cells cannot be reversed although it is often possible to prevent further damage. This damage can progress until only central vision is left or until the person is completely blind. The longer the disease is left untreated, the greater the damage. Modern examination techniques and treatment have made Glaucoma a rare cause of blindness in Australia.
How can I tell if I have Glaucoma?
Often you will not be aware that you have Glaucoma until it is too late. Usually there are no symptoms until permanent damage has occurred. In some cases the increased pressure in the eye will cause blurred vision, apparent coloured rings around lights, loss of side vision, and pain and redness of the eye.
How does an optometrist diagnose Glaucoma?
To diagnose Glaucoma the optometrist looks at the nerve fibres at the back of the eye, examines the eye’s drainage network and measures the pressure in the eye with a special instrument called a tonometer. If your optometrist suspects glaucoma, they will perform a peripheral vision test (visual field examination) and OCT (Optical Coherence Tomography). These tests are simple and painless.
How is Glaucoma treated?
Eye drops and medicine are often used to treat Glaucoma initially. Surgery may be necessary if the blockage in the drainage system cannot be removed in other ways. Your optometrist will refer you to an eye specialist for treatment if they suspect you have Glaucoma.
Can Glaucoma be prevented?
No. Early detection and treatment is the best way to control Glaucoma.
Who is likely to be affected by Glaucoma?
People over the age of 40 years are far more likely to have Glaucoma than younger people. Also, Glaucoma tends to run in families. People with a blood relative who has suffered from Glaucoma and people over 40 years of age are at risk and should have their eyes checked regularly by an optometrist.
Keratoconus
Keratoconus
What is Keratoconus?
Keratoconus (literally, ‘conical cornea’) is a thinning and steepening of the cornea, the front clear window of the eye. As the cornea thins, the normal pressure within the eye makes the thinner area of the cornea bulge forward slightly.
Keratoconus can be an inherited disorder but may also happen in individuals without any family history of the condition. It occurs in about one in 3000 people. The condition usually becomes apparent between the ages of 10 and 25 years, and is sometimes associated with other conditions such as allergies, infantile eczema, asthma, reduced night vision, double jointedness, and in rare instances, with occasional short bouts of chest pain.
Because keratoconus is a genetic condition it cannot be treated with drugs, but glasses and contact lenses can improve vision, and surgery can be used to treat progressive or severe cases. Keratoconus does not cause blindness. Interestingly, about 60 per cent of people with keratoconus go on to tertiary education, compared with 15 per cent of the population as a whole.
The initial symptoms of keratoconus are blurred vision, caused by short-sightedness and astigmatism. These are caused by the cornea changing shape as it bulges forward, and are often indistinguishable from shortsightedness caused by other factors. At this stage, good vision generally can be obtained with spectacles.
As keratoconus progresses, the shape of the cornea becomes irregular, and it is not possible to correct the vision with spectacles alone. In such cases, rigid contact lenses can be used to provide good vision. The contact lenses essentially provide a new, regular front surface for the eye, eliminating the distortions caused by the keratoconus.
Because the cornea continues to change shape, it is important that people with keratoconus have regular eye examinations to ensure that their contact lenses fit correctly. A poorly fitting contact lens can cause abrasions and scarring.
In approximately 85 per cent of cases of keratoconus the condition gradually stabilizes by the age of 35 years, although exceptions are always possible. In the remaining 15 per cent the condition progresses, and vision and tolerance to contact lenses may deteriorate. For anyone with progressive keratoconus, intervention with a relatively new surgical procedure called Collagen Cross Linking may stabilize the cornea and even halt progression. If your keratoconus is progressing, your optometrist will discuss this surgical option with you and refer you to an ophthalmologist.
In late uncontrolled stages of the disease a corneal graft may be necessary. A corneal graft or keratoplasty is an operation in which the thinned area of the cornea is removed and replaced by normal tissue transplanted from a donor cornea. Corneal grafting is used only when all other methods for correcting vision have failed to provide good vision. The success rate for corneal grafts is extremely high, although most people will still need to wear glasses or contact lenses.
Macula Degeneration
Macula Degeneration
What is age-related Macular Degeneration?
Age-related Macular Degeneration (ARMD), also known as senile macular degeneration, is damage or breakdown of the macula. The macula is a very small part of the retina, the light-sensitive tissue of the eye, which is responsible for central vision. This is the part of the retina that produces the finest detailed vision.
How does Macular Degeneration affect vision?
As Macular Degeneration damages the part of the retina responsible for central vision and for seeing fine detail, it becomes difficult to see small details of objects. Vision to the sides is not affected. If both eyes are affected, reading and other tasks requiring fine vision may become very difficult. Macular Degeneration does not cause blindness. Because some side vision remains, usually people can still take care of themselves.
What causes Macular Degeneration?
Macular Degeneration is the result of ageing processes in the eye. Some of the layers of the retina thicken and waste material which is usually removed from the retina forms deposits, distorting the retina. This distortion can cause damage to the other layers of the retina. In about 10 per cent of cases, new blood vessels grow into the macula from beneath. These newly-formed vessels are fragile and often leak blood into the retina where the blood causes scar tissue to form. The scarring blocks out central vision to a severe degree. There are also some other forms of macular degeneration which are inherited and not associated with ageing.
How common is Macular Degeneration?
Macular Degeneration mainly affects older people: about four per cent of those more than 40 years old, nine per cent of those over 50 years, 23 per cent of those over 65 years and 31 per cent of those aged 80 years or more. Men and women are equally affected. Macular Degeneration accounts for up to 45 per cent of legal blindness and up to 70 per cent of seriously impaired vision in people over the age of 70 years.
How is Macular Degeneration detected and diagnosed?
People with Macular Degeneration may notice that their vision has deteriorated. Many patients do not realise that they have a problem until their vision becomes blurred. Optometrists perform a number of tests in an examination which enables them to detect the presence of Macular Degeneration in the early stages. The optometrist examines the macula carefully and takes digital pictures of the macular so that any changes can be precisely visible. Sometimes the optometrist may place a drop in the eye to dilate the pupil to get a better view of the internal structures. Through techniques called fundoscopy or ophthalmoscopy the optometrist will look for changes in the structure of the macula such as accumulations of waste material or new blood vessels. Another test that may be used is a grid pattern known as an Amsler chart. This is a regular grid which looks like a piece of graph paper. Patients with Macular Degeneration often report that sections of the grid appear to be distorted or missing.
Some types of severe Macular Degeneration need to be monitored by an ophthalmologist (eye surgeon). Your optometrist will refer you if you have this form and the ophthalmologist may perform a test called fluorescein angiography. In this test a fluorescent dye is injected into the patient’s bloodstream and the ophthalmologist observes the progress of the dye through the blood vessels in the retina. This reveals any leaking blood vessels.
Can Macular Degeneration be treated?
When most body tissues such as a muscle, skin or bone are damaged, the tissues’ cells have the capacity to regrow and repair the damage. Because nerve cells cannot regenerate, damage to nerve tissue, such as the retina, is usually permanent and irreversible. This is why the vision loss in Macular Degeneration is so difficult to treat, compared with other vision disorders. For example, it is possible to remove and replace the eye’s lens in a person with cataract but it is not possible to replace or even repair the retina of a person with Macular Degeneration.
One possible management which has been shown to decrease the likelihood of macula degeneration worsening in some people who already suffer with the disease include vitamins. A large study (AREDS 2) found that a specific combination of Vitamins could reduce the likliehood of the degeneration progressing. Ask your optometrist about whether you may be helped by this treatment.
In cases where new blood vessels have appeared in the macula area, laser surgery or injections may be used. In laser treatment a focused, intense beam of laser light is used to seal off leaking blood vessels and to prevent new vessels growing. There are also eye injections that may slow or prevent the formation of new blood vessels. These treatments are most effective when applied in the very early stages of the disease, before extensive damage has been done.
While there is little which can be done to prevent or cure Macular Degeneration, people with the disease can be helped to continue functioning normally. Many patients with Macular Degeneration will eventually come under the classification of being a low vision patient. Special help in the form of low vision devices is available from optometrists and specialist low vision clinics. Low vision devices enable patients to make the most of their vision and include items such as miniature telescopes, high-powered reading spectacles, hand-held and stand magnifiers, closed circuit televisions and other simpler aids such as large-print books.
What should you do about Macular Degeneration?
For treatment of Macular Degeneration to be effective, it must be diagnosed as early as possible. Regular eye examinations are the key to early detection of retinal changes and other signs of disease. If you notice any change in the quality of your vision, have your eyes examined immediately. Regular examinations are particularly important for people over the age of 50 years and people whose families have a history of eye problems.
Pterygium
Pterygium
What is a Pterygium?

A Pterygium (pronounced te-ri-gi-um, plural: Pterygia) is a triangular-shaped lump of tissue which grows from the conjunctiva (the thin membrane which covers the white of the eye) on to the cornea (the clear central part of the eye). Pterygia often occur in both eyes, usually on the side of the eye closer to the nose. A Pterygium is not a cancer. People sometimes confuse Pterygia with Cataracts. A Cataract is a clouding of the lens inside the eye and cannot be seen easily with the naked eye.
What causes Pterygia?
The exact causes of Pterygia are not known, but they are strongly associated with exposure to ultraviolet radiation and hot, dry environments. Pterygia are more common in the Northern parts of Australia and among people such as farmers and surfers who spend a lot of time outdoors, but anyone can develop a Pterygium.
Are Pterygia dangerous?
Pterygia are not dangerous, although they can look unpleasant and cause some discomfort. The main problem with Pterygia is that as they grow onto the cornea they distort it, interfering with vision. If the Pterygium grows on to the central part of the cornea it can begin to block light from entering the eye. This can cause vision loss.
Although a Pterygium is not dangerous, it should be checked to make sure that it is not something more serious and that it is not progressing. If you have any area of tissue on or around the eyes that changes rapidly you should consult an optometrist or eye surgeon (ophthalmologist) immediately.
How can Pterygia be treated?
In cases where the Pterygium is not actively growing on to the cornea, protecting the eyes from ultraviolet light often will stabilise its growth. In many cases, provided it is not threatening vision and it remains stable, this may be all that is required. In cases where the Pterygium is actively growing on to the cornea and threatening to distort the vision, the only effective treatment is surgical removal. Fortunately this is relatively minor surgery that usually is performed under a local anaesthetic.
It is best to have surgery before the Pterygium progresses to the point where it interferes with vision. Your optometrist can assess the Pterygium and refer you to an eye surgeon if it requires removal.
How can Pterygia be prevented?
The best way to reduce your risk of developing a Pterygium is to protect your eyes from ultraviolet light. UV radiation can also cause Cataracts and other eye diseases, as well as skin cancers, so reducing exposure is a wise move. The best ways of doing this are to:
- Avoid the sun: in summer, three-quarters of outdoors UV exposure occurs between 10 am and 4pm. Staying out of the sun between those times will significantly reduce your UV exposure.
- Wear a hat: a broad-brimmed hat will not only protect your head from sunburn, but will reduce by at least half the amount of UV radiation reaching your eyes.
- Wear sunglasses: a good pair of sunglasses will reduce the amount of UV reaching your eyes and cut the amount of glare. Wrap-around sunglasses are best as they block UV radiation that can slip around the sides of conventional sunglasses.
Eye Conditions
Normal Vision
Normal Vision
For perfect clear vision, what we see (an image) needs to be focused onto the retina, just like a camera has to be focused properly in order to take a clear picture.
If the image is not focused exactly on the retina, then the image will be blurred, just like an out-of-focus photograph. In this case, the person is said to have a refractive error.
Refractive errors occur when there is a mismatch between the length of the eye, and its optical power. These mismatches usually originate during childhood, when the eyes are growing. The exact causes of refractive errors are still being studied, but it is known that both hereditary and environmental influences can affect their development.
Most people have some refractive error, but in most cases the error is small, and does not cause any problems. Above the age of 40, it is normal for the near reading vision to become slightly blurred. This is due to presbyopia.
Myopia
Myopia | Short Sightedness
What is Myopia?
Myopia is what most people call short-sightedness. Short-sighted people do not see distant objects clearly. The eye’s lens and cornea normally focus light into an image on the retina. In a myopic eye the light is focused in front of the retina and so the image is blurred.
Does a short-sighted person see close objects more clearly than a person with normal vision?
No. Short-sighted people see close objects equally as well or sometimes slightly worse. When their myopia is corrected, they see objects equally as well.
How can I tell if I am shortsighted?
Shortsighted people have difficulty in seeing distant objects clearly. They find it hard to read road signs and scoreboards. Recognising people in the distance and playing ball games also may be a problem for many short-sighted people. Often a person will not realise that they cannot see clearly but an eye examination by an optometrist will reveal the problem.
How can I tell if my child is shortsighted?
A complete eye test is the only sure way of determining whether your child’s vision is normal. Some clues to myopia in a child are:
- Squinting eyes to see distant objects.
- Difficulty in reading the blackboard at school.
- Poor posture while reading.
- Lack of interest in playing outdoor games.
What causes Myopia?
Myopia is caused by a mismatch between the power of the optical components of the eye and the length of the eye (the ‘axial length’). Either the power is too high, or the length is too long, or both. Usually the cornea (the front surface of the eye) is curved more steeply than average, increasing its optical power. The exact causes of the mismatch between power and axial length are unknown. There is some genetic influence (if your parents are short-sighted, you have a greater chance of being short-sighted yourself), and there is some evidence for environmental factors, such as excessive amounts of near work, having some influence.
Can Myopia be cured?
No, but properly prescribed spectacles or contact lenses will enable the person to see clearly. The lenses diverge incoming light rays, so that they will be properly focused on the retina. There are also a number of techniques available for re-shaping the cornea (the front surface of the eye), in order to reduce its power and thus correct the myopia. One technique (known as orthokeratology or ‘Ortho-K’) uses rigid contact lenses to change the shape of the cornea while you sleep so that you can be free of contact lenses and glasses during the day. Other surgical techniques use lasers or implants to change the power of the front of the eye.
Can Myopia be prevented?
There is no certain prevention for myopia. However, in some cases, treatment can be prescribed to stop or slow its progression.
Recent research indicates that lowered rates of myopia are linked with outdoor activity of 10-14 hours per week. One thought as to why outdoor activity at a young age can reduce myopia progression is that sunlight stimulates retinal dopamine. This in turn inhibits eye growth and therefore also myopia.
How common is Myopia?
It is a very common condition. With approximately 15% of the population being short-sighted. Usually myopia starts to develop in teenage years and may get worse in early adulthood.
Can Myopia cause other problems?
High levels of myopia can cause other, more serious problems. People with high levels of myopia often have very large, elongated eyes, and their retinas may be stretched and thinner than normal. This increases the risk of the retina developing holes and tears and the risk of retinal detachments. If you are myopic you should have regular eye examinations, and talk to your optometrist about the potential for problems.
Astigmatism
Astigmatism
What is Astigmatism?
Astigmatism is a focusing error that causes asymmetric blur. Some directions in an image are more out of focus than others. This can be contrasted with short-sightedness (Myopia) where all directions are uniformly blurred.
What does it look like?
Astigmatism causes different amounts of blur in different directions. This causes images to appear distorted, or sometimes even double. Certain letters may be more difficult to read than others, depending on the orientation of the lines within them.
One type of chart used to detect Astigmatism uses a series of lines arranged in a fan shape – if you have Astigmatism, some lines will appear clearer than others.
What causes Astigmatism?
Most Astigmatism is caused by the irregular shape of the front surface of the eye (the cornea). It can also be caused by slight tilting of the lens inside the eye. It may be an inherited characteristic or a normal variation accompanying growth.
Can you describe the shape?
A magnifying glass focuses the sun to a point image because its two surfaces are spherical, each like the surface of a basketball. Now imagine a transparent surface shaped like the side of an Australian Rules or rugby football. It has two different curvatures. These result in light focusing at two different locations. The image does not focus to a point and so is blurred.
How does Astigmatism affect me?
Objects at all distances are indistinct or blurred and the eye cannot focus. Even slight degrees of astigmatism may encourage headaches, fatigue and reduce concentration. The eyes may try, without success, to correct the blur. There is also a tendency to squint the eyes to try to see better, producing discomfort in the muscles of the eyelid and face.
How is Astigmatism corrected?
Spectacles and contact lenses (hard and soft) can correct Astigmatism. Sometimes correction of Astigmatism can cause a change in the apparent size and shape of objects and may affect judgment of distance. A patient may feel taller or shorter or see objects appearing to slope and curve.
In most cases, adjustment to these side effects takes only a week or so. Astigmatism correction may involve a compromise between optimal clarity and visual discomfort.
How is Astigmatism detected?
Some people notice blur themselves. Only a proper eye examination will determine for certain if you have Astigmatism. Astigmatism is not an eye disease and any changes are generally gradual and not necessarily for the worse. Most people have at least very slight Astigmatism.
Colour Vision Deficiency
Colour Vision Deficiency
What is Colour Vision Deficiency?
Colour vision defects are almost always inherited, although some forms can be an acquired condition as a result of some diseases or injuries.
The abnormality is sex linked, recessive, and carried on the X chromosomes. Males have one X chromosome and females have two. In relation to colour defects, this means that any males that have a defect on their one X chromosome will exhibit a colour vision defect, while females must carry the same type of colour vision defect on both their X chromosomes to be colour vision deficient. If females have it only on one X chromosome they will carry the condition but still have normal colour vision themselves.
In the general population, about 8% of males and 0.5% of females have colour vision deficiencies. Almost all colour deficient people do see a large range of colours but they will have difficulty identifying particular colours. The most common defects lead to confusing certain shades of red and green for example.
As children, few of these people will be aware that they have a colour vision deficiency but the detection of these problems is important, especially when career choices are affected.
See Below for an example of an Ishihara Colour Vision Examination Plate:
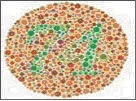
A colour vision assessment can be carried out by one of our qualified optometrists.
Presbyopia
Presbyopia
What is Presbyopia?
Presbyopia is a common condition that makes vision difficult at a normal reading distance. It is not a disease.
How will Presbyopia affect my vision?

Initially, close tasks such as reading and sewing become difficult, particularly under poor lighting conditions. Later, even tasks further away such as laptop or computer use may become difficult. For example, initially you may find that you are holding your newspaper further away from your eyes to make the print clearer. Presbyopia does not affect distance vision. You may also have difficulty concentrating when reading, or you may find periods of close work result in sore eyes, headaches or tiredness.
What causes Presbyopia?
It is important to understand how your eyes change their focus for viewing close objects. Normally they are focused for distance vision. Inside the eye there is a lens about the size of a pea. To focus on close objects, a special muscle in the eye changes the shape of the lens. This process is called accommodation.
With age the lens loses its flexibility and is less able to change its shape. This is a completely normal ageing change, just like stiffening joints or greying hair. The loss in lens flexibility is the reason that close focusing becomes more difficult.
Who is likely to become presbyopic?
Everyone experiences the ageing process that causes presbyopia. The condition cannot be prevented.
Does Presbyopia come on quickly?
No. Presbyopia is usually first noticed around the age of 40 to 45 years. Although difficulties with close work may seem to come on suddenly, the ageing process that causes presbyopia is gradual and has been going on since childhood. Between the ages of 45 and 65 the amount of presbyopia increases, making near work more difficult. From 65 years onwards, there are unlikely to be any further significant changes to vision due to presbyopia.
How is Presbyopia treated?
Presbyopia is corrected with either spectacles or contact lenses with a prescription designed especially for close distances. It is important that the prescription is calculated for the distance at which you do your close tasks.
Discussion with your optometrist will help to determine the best way of preparing your prescription. The correction for presbyopia will make near objects clear but distant objects blurry. This means that if you have a pair of spectacles just for reading you will not be able to watch television while wearing them.
Having different prescriptions for distance and reading can be a nuisance, especially if you have to change spectacles all the time. One way around the problem is the use of a multifocal. These are special lenses that have a prescription for distance vision in the top half of the lens and a gradual progression in power to the reading prescription in the lower half.
Does Presbyopia mean that my eyes are deteriorating?
No. Although your close focusing system is not functioning as well as it used to, once Presbyopia has been corrected with spectacles you will be able to see close things as well as you always did. Presbyopia does not represent a threat to your eyes’ health.
When should I have my prescription for Presbyopia renewed?
Between the ages of 45 and 65 your prescription is likely to change significantly. Its recommended to have your eyes examined every two years to review your prescription and your general eye health. If you experience vision problems within two or three years of your previous examination you should make a review appointment with your optometrist. Your optometrist will advise you of the most appropriate period between consultations.
Will wearing spectacles weaken my eyes?
No. Presbyopia will continue regardless of whether spectacles are worn. Wearing spectacles will not accelerate or slow the development of Presbyopia.
Eye Diseases
Cataracts
Cataracts

What are Cataracts?
Cataracts are cloudy areas that form in the lens of the eye. The lens is normally clear. Poor vision results because the cloudiness interferes with light entering the eye. The opacities in the lens scatter the light, causing hazy vision, in the same way that a dirty window scatters light and is more difficult to see through.
Are Cataracts a kind of growth?
No. Cataracts are due to a change in the lens material, they are not an extra part growing within the eye. Cataracts can become worse as more of the previously normal lens material changes.
What causes Cataracts?
Most Cataracts are a result of ageing and long-term exposure to ultraviolet light. Some are caused by injury and certain diseases and in rare cases by exposure to toxic materials and radiation. Occasionally Cataracts are present at birth, this can be due to the baby’s mother having had rubella during the pregnancy, or be a genetic defects.
Do Cataracts get worse?
Yes. The clouded areas become larger and denser and cause sight to become worse. The time taken for this to happen varies from a few months to many years.
Do Cataracts affect both eyes?
Usually Cataracts affect both eyes but often develop at different rates in each eye.
How common are Cataracts?
People older than 65 years often have signs of Cataracts and should have their eyes examined regularly. The severity of cataract varies considerably between individuals of the same age.
Can Cataracts cause blindness?
If untreated, Cataracts can cause blindness. Blindness can be prevented by detecting the Cataracts early and, if necessary, by having them removed surgically. Your optometrist will refer you to an eye specialist if they consider that you need surgical treatment for your Cataracts.
How well will I see if my lens is removed?
In most cases very well. Most patients have an intra-ocular lens (IOL) inserted at the time of surgery, with excellent results. This is a clear plastic lens that replaces your own cloudy one. Patients may still need to wear spectacles or contact lenses after surgery.
What are the signs of Cataracts?
Usually the development of Cataracts is gradual with a painless worsening of sight. Other symptoms include blurred or hazy vision, spots before the eyes, double vision and a marked increase in sensitivity to glare.
How can I be sure I don’t have Cataracts?
An examination by your optometrist will reveal any changes that have occurred in the lens of the eye. Optometrists have special equipment that enables them to see changes in the lens that may lead to Cataracts several years before any symptoms appear.
Can Cataracts be prevented?
There is no proven method of preventing Cataracts. Long-term exposure to ultraviolet light is thought to induce Cataracts, so a brimmed hat and Australian approved sunglasses should be worn in sunlight.
When should I have a Cataract operation?
This varies with each patient. Usually cataract surgery is performed when the patient’s vision interferes with their daily life. Your optometrist will assist you in making this decision.
Is Cataract removal a major operation?
Cataract surgery is now a relatively minor procedure. Often it is performed under a local anaesthetic. Depending on the patient, the surgery may be performed on an out-patient basis. This means that the patient attends a hospital or clinic for the surgery and is able to go home the same day. The surgery is performed by an ophthalmologist, a medical doctor who specialises in eye surgery. Your optometrist will refer you to an ophthalmologist when necessary.
Conjunctivitis
Conjunctivitis

What is conjunctivitis?
Conjunctivitis is an inflammation of the conjunctiva, the thin, transparent layer covering the surface of the inner eyelid and a portion of the front of the eye. This condition appears in many forms and affects people of all ages.
What causes conjunctivitis?
The three main types of conjunctivitis are infectious, allergic and chemical. The infectious form, commonly known as “pink eye” is caused by a contagious virus or bacteria. Your body’s allergies to pollen, cosmetics, animals or fabrics can often bring on allergic conjunctivitis. And, irritants like air pollution, noxious fumes and chlorine in swimming pools may produce the chemical form.
What are the signs/symptoms of conjunctivitis?
Common signs/symptoms of conjunctivitis are red eyes, inflamed inner lids, watery eyes, blurred vision and a sandy or scratchy feeling in the eyes. With the infectious form, there may be a puss-like or watery discharge around the eyelids. Since infectious conjunctivitis is contagious, measures should be taken to prevent spreading this condition. To avoid giving infectious conjunctivitis to others, keep your hands away from your eyes; thoroughly wash your hands before and after applying eye medication; do not share towels, flannels, cosmetics or eyedrops with others and seek treatment promptly. Small children, who may forget these precautions, should be kept away from school and the swimming pool until the condition is cured.
Diabetes
Diabetes
Diabetes and Diabetic Retinopathy
What is Diabetic Retinopathy?
Patients with diabetes are more likely to develop eye problems such as cataracts and glaucoma, but the disease’s affect on the retina is the main threat to vision. Most patients develop diabetic changes in the retina after approximately 15 years of the disease. The effect of diabetes on the retina is called diabetic retinopathy.
In this condition the small blood vessels in the retina become weakened and leak, forming small hemorrhages. The leaking of the vessels often leads to swelling in the retina and decreased vision. If untreated circulation problems can occur in these vessels and the retina becomes deprived of oxygen. This leads to death of the cells in the retina and a permanent loss of vision.
If you are diabetic the National Health and Medical Research Council recommends yearly dilated eye examinations so that related eye problems can be detected and treated as early as possible. At our practice we perform detailed dilated fundus examinations on all diabetics. We communicate with your general practitioner (GP) and also ophthalmologists (Eye specialists) to give you the best possible care.
There are two main types of this condition: background retinopathy and proliferative retinopathy. The risk of developing retinopathy increases with the length of time you have had diabetes. The risk is also increased by poor control of blood sugar levels and blood pressure levels.
Background Retinopathy
This is the more mild form of diabetic retinopathy. This may involve hemorrhages and leaking blood vessels. More serious complications include swelling of the retina which may cause vision loss. This stage of retinopathy indicates that the blood sugar levels are not within appropriate levels.
Proliferative Retinopathy
This condition is more serious and requires early treatment to prevent serious vision loss. Your optometrist can recognise signs that this condition might develop, or detect it in its early stages. Once proliferative retinopathy has been diagnosed, your optometrist will refer you to an eye surgeon for further appraisal and probable laser treatment. Treatment of this condition has a better chance of success if it is applied very early.
Managing Diabetic Retinopathy
The time at which diabetic retinopathy begins is not predictable. Some people can have diabetic retinopathy upon being diagnosed with diabetes and others will have no signs of retinopathy even 15 years after being diagnosed with diabetes. The best management is to have regular eye examinations so that changes can be detected and treated early. It is advisable for all people with diabetes to have yearly eye examinations. People who have been diagnosed as having retinopathy should have eye examinations more frequently than once a year.
Diabetes and other vision conditions:
Double vision
This is a distressing but rare complication of diabetes. The condition is usually temporary but it may last for a few months. An optometrist can help treat it while it has effect. Diabetes is not the only cause of double vision.
Glaucoma
The eye disease Glaucoma is slightly more common in diabetic people than in the general community. Glaucoma is a condition in which the nerve cells that transmit information from the eye to the brain become damaged, often caused by pressure due to a build-up of fluid in the eye. If untreated, Glaucoma can cause blindness.
Cataract
Cataracts are more likely to occur in diabetic people at an earlier age than in non-diabetic people. A cataract is a cloudiness that can form in the lens inside the eye. If present, Glaucoma and cataract will be readily detected at your regular eye examination when your optometrist will advise the best management strategy for the condition.
Dry Eye
Dry Eye
What is “Dry Eye?”
The tears your eyes normally produce are necessary for overall eye health and clear vision. Dry eye occurs when your eyes do not produce enough tears or produce tears which do not have the proper chemical composition.
What causes Dry Eye?
Dry eye symptoms can result from the normal ageing process, exposure to environmental conditions, problems with normal blinking or from medications such as antihistamines, oral contraceptives or antidepressants. Dry eye can also be symptomatic of general health problems, other diseases or can result from chemical or thermal burns to the eye.
What are the Signs/Symptoms of Dry Eye?
The most common signs/symptoms include burning, stinging, itchy, scratchy, gritty and uncomfortable eyes. You may experience increased dry eye symptoms on waking. Some people experience watering eyes. This is a natural reflex to comfort a dry eye.
How is Dry Eye diagnosed?
During the examination, your optometrist will ask you questions about your eye comfort, general health, your use of medications and your home and work environments to determine any factors which may be causing dry eye symptoms. This information will help us to decide whether to perform dry eye tests. These tests allow your optometrist to evaluate the quality, the amount and the distribution of tears to detect signs of dry eyes.
Can Dry Eye be cured?
Dry eye cannot be cured, but your eyes’ sensitivity can be lessened and measures taken so your eyes remain healthy. The most frequent treatment is the use of artificial tears or tear substitutes. For more severe dry eye, ointment can be used, especially at bedtime. Other treatments involve warm eyelid compresses and massage. In some cases, small plugs may be inserted in the corner of the eyelids to slow drainage and loss of tears.
Will Dry Eye harm my eyes?
If dry eye is untreated, it can harm your eyes. Excessive dry eye can damage tissue and possibly scar the cornea of your eye, impairing vision. Dry eye can make contact lens wear more difficult due to increased irritation and a greater chance of eye infection. To keep dry eye symptoms in check, you and your optometrist need to work together.
If you have increased dryness or redness that is not relieved by the prescribed treatment, let us know as soon as possible.
If you continue to have discomfort, the drops may be used more frequently or as needed. You should return for follow-up care as recommended.
Glaucoma
Glaucoma
What is Glaucoma?

Glaucoma is a condition in which the nerve cells that transmit information from the eye to the brain become damaged. This prevents visual information from getting from the retina in the eye to the brain. Glaucoma is often linked with a build up of pressure in the eye. The eye is filled with fluid that is constantly being replaced. If excessive amounts of fluid are produced, or if it cannot drain away properly, the pressure inside the eye can increase. In some forms of Glaucoma, the pressure inside the eye can become extremely high, but in other forms the pressure may remain normal.
What causes Glaucoma?
The exact causes of Glaucoma are not known. In some cases the drainage network of the eye may not be formed properly, or may become blocked by natural materials or due to injury; in other cases there is no clear cause.
Is the damage that occurs in Glaucoma serious?
If untreated, Glaucoma can cause blindness. As the nerve cells are progressively damaged, the ability to see objects in different parts of the visual field and your peripheral vision is lost. The damage to the nerve cells cannot be reversed although it is often possible to prevent further damage. This damage can progress until only central vision is left or until the person is completely blind. The longer the disease is left untreated, the greater the damage. Modern examination techniques and treatment have made Glaucoma a rare cause of blindness in Australia.
How can I tell if I have Glaucoma?
Often you will not be aware that you have Glaucoma until it is too late. Usually there are no symptoms until permanent damage has occurred. In some cases the increased pressure in the eye will cause blurred vision, apparent coloured rings around lights, loss of side vision, and pain and redness of the eye.
How does an optometrist diagnose Glaucoma?
To diagnose Glaucoma the optometrist looks at the nerve fibres at the back of the eye, examines the eye’s drainage network and measures the pressure in the eye with a special instrument called a tonometer. If your optometrist suspects glaucoma, they will perform a peripheral vision test (visual field examination) and OCT (Optical Coherence Tomography). These tests are simple and painless.
How is Glaucoma treated?
Eye drops and medicine are often used to treat Glaucoma initially. Surgery may be necessary if the blockage in the drainage system cannot be removed in other ways. Your optometrist will refer you to an eye specialist for treatment if they suspect you have Glaucoma.
Can Glaucoma be prevented?
No. Early detection and treatment is the best way to control Glaucoma.
Who is likely to be affected by Glaucoma?
People over the age of 40 years are far more likely to have Glaucoma than younger people. Also, Glaucoma tends to run in families. People with a blood relative who has suffered from Glaucoma and people over 40 years of age are at risk and should have their eyes checked regularly by an optometrist.
Keratoconus
Keratoconus
What is Keratoconus?
Keratoconus (literally, ‘conical cornea’) is a thinning and steepening of the cornea, the front clear window of the eye. As the cornea thins, the normal pressure within the eye makes the thinner area of the cornea bulge forward slightly.
Keratoconus can be an inherited disorder but may also happen in individuals without any family history of the condition. It occurs in about one in 3000 people. The condition usually becomes apparent between the ages of 10 and 25 years, and is sometimes associated with other conditions such as allergies, infantile eczema, asthma, reduced night vision, double jointedness, and in rare instances, with occasional short bouts of chest pain.
Because keratoconus is a genetic condition it cannot be treated with drugs, but glasses and contact lenses can improve vision, and surgery can be used to treat progressive or severe cases. Keratoconus does not cause blindness. Interestingly, about 60 per cent of people with keratoconus go on to tertiary education, compared with 15 per cent of the population as a whole.
The initial symptoms of keratoconus are blurred vision, caused by short-sightedness and astigmatism. These are caused by the cornea changing shape as it bulges forward, and are often indistinguishable from shortsightedness caused by other factors. At this stage, good vision generally can be obtained with spectacles.
As keratoconus progresses, the shape of the cornea becomes irregular, and it is not possible to correct the vision with spectacles alone. In such cases, rigid contact lenses can be used to provide good vision. The contact lenses essentially provide a new, regular front surface for the eye, eliminating the distortions caused by the keratoconus.
Because the cornea continues to change shape, it is important that people with keratoconus have regular eye examinations to ensure that their contact lenses fit correctly. A poorly fitting contact lens can cause abrasions and scarring.
In approximately 85 per cent of cases of keratoconus the condition gradually stabilizes by the age of 35 years, although exceptions are always possible. In the remaining 15 per cent the condition progresses, and vision and tolerance to contact lenses may deteriorate. For anyone with progressive keratoconus, intervention with a relatively new surgical procedure called Collagen Cross Linking may stabilize the cornea and even halt progression. If your keratoconus is progressing, your optometrist will discuss this surgical option with you and refer you to an ophthalmologist.
In late uncontrolled stages of the disease a corneal graft may be necessary. A corneal graft or keratoplasty is an operation in which the thinned area of the cornea is removed and replaced by normal tissue transplanted from a donor cornea. Corneal grafting is used only when all other methods for correcting vision have failed to provide good vision. The success rate for corneal grafts is extremely high, although most people will still need to wear glasses or contact lenses.
Macula Degeneration
Macula Degeneration
What is age-related Macular Degeneration?
Age-related Macular Degeneration (ARMD), also known as senile macular degeneration, is damage or breakdown of the macula. The macula is a very small part of the retina, the light-sensitive tissue of the eye, which is responsible for central vision. This is the part of the retina that produces the finest detailed vision.
How does Macular Degeneration affect vision?
As Macular Degeneration damages the part of the retina responsible for central vision and for seeing fine detail, it becomes difficult to see small details of objects. Vision to the sides is not affected. If both eyes are affected, reading and other tasks requiring fine vision may become very difficult. Macular Degeneration does not cause blindness. Because some side vision remains, usually people can still take care of themselves.
What causes Macular Degeneration?
Macular Degeneration is the result of ageing processes in the eye. Some of the layers of the retina thicken and waste material which is usually removed from the retina forms deposits, distorting the retina. This distortion can cause damage to the other layers of the retina. In about 10 per cent of cases, new blood vessels grow into the macula from beneath. These newly-formed vessels are fragile and often leak blood into the retina where the blood causes scar tissue to form. The scarring blocks out central vision to a severe degree. There are also some other forms of macular degeneration which are inherited and not associated with ageing.
How common is Macular Degeneration?
Macular Degeneration mainly affects older people: about four per cent of those more than 40 years old, nine per cent of those over 50 years, 23 per cent of those over 65 years and 31 per cent of those aged 80 years or more. Men and women are equally affected. Macular Degeneration accounts for up to 45 per cent of legal blindness and up to 70 per cent of seriously impaired vision in people over the age of 70 years.
How is Macular Degeneration detected and diagnosed?
People with Macular Degeneration may notice that their vision has deteriorated. Many patients do not realise that they have a problem until their vision becomes blurred. Optometrists perform a number of tests in an examination which enables them to detect the presence of Macular Degeneration in the early stages. The optometrist examines the macula carefully and takes digital pictures of the macular so that any changes can be precisely visible. Sometimes the optometrist may place a drop in the eye to dilate the pupil to get a better view of the internal structures. Through techniques called fundoscopy or ophthalmoscopy the optometrist will look for changes in the structure of the macula such as accumulations of waste material or new blood vessels. Another test that may be used is a grid pattern known as an Amsler chart. This is a regular grid which looks like a piece of graph paper. Patients with Macular Degeneration often report that sections of the grid appear to be distorted or missing.
Some types of severe Macular Degeneration need to be monitored by an ophthalmologist (eye surgeon). Your optometrist will refer you if you have this form and the ophthalmologist may perform a test called fluorescein angiography. In this test a fluorescent dye is injected into the patient’s bloodstream and the ophthalmologist observes the progress of the dye through the blood vessels in the retina. This reveals any leaking blood vessels.
Can Macular Degeneration be treated?
When most body tissues such as a muscle, skin or bone are damaged, the tissues’ cells have the capacity to regrow and repair the damage. Because nerve cells cannot regenerate, damage to nerve tissue, such as the retina, is usually permanent and irreversible. This is why the vision loss in Macular Degeneration is so difficult to treat, compared with other vision disorders. For example, it is possible to remove and replace the eye’s lens in a person with cataract but it is not possible to replace or even repair the retina of a person with Macular Degeneration.
One possible management which has been shown to decrease the likelihood of macula degeneration worsening in some people who already suffer with the disease include vitamins. A large study (AREDS 2) found that a specific combination of Vitamins could reduce the likliehood of the degeneration progressing. Ask your optometrist about whether you may be helped by this treatment.
In cases where new blood vessels have appeared in the macula area, laser surgery or injections may be used. In laser treatment a focused, intense beam of laser light is used to seal off leaking blood vessels and to prevent new vessels growing. There are also eye injections that may slow or prevent the formation of new blood vessels. These treatments are most effective when applied in the very early stages of the disease, before extensive damage has been done.
While there is little which can be done to prevent or cure Macular Degeneration, people with the disease can be helped to continue functioning normally. Many patients with Macular Degeneration will eventually come under the classification of being a low vision patient. Special help in the form of low vision devices is available from optometrists and specialist low vision clinics. Low vision devices enable patients to make the most of their vision and include items such as miniature telescopes, high-powered reading spectacles, hand-held and stand magnifiers, closed circuit televisions and other simpler aids such as large-print books.
What should you do about Macular Degeneration?
For treatment of Macular Degeneration to be effective, it must be diagnosed as early as possible. Regular eye examinations are the key to early detection of retinal changes and other signs of disease. If you notice any change in the quality of your vision, have your eyes examined immediately. Regular examinations are particularly important for people over the age of 50 years and people whose families have a history of eye problems.
Pterygium
Pterygium
What is a Pterygium?

A Pterygium (pronounced te-ri-gi-um, plural: Pterygia) is a triangular-shaped lump of tissue which grows from the conjunctiva (the thin membrane which covers the white of the eye) on to the cornea (the clear central part of the eye). Pterygia often occur in both eyes, usually on the side of the eye closer to the nose. A Pterygium is not a cancer. People sometimes confuse Pterygia with Cataracts. A Cataract is a clouding of the lens inside the eye and cannot be seen easily with the naked eye.
What causes Pterygia?
The exact causes of Pterygia are not known, but they are strongly associated with exposure to ultraviolet radiation and hot, dry environments. Pterygia are more common in the Northern parts of Australia and among people such as farmers and surfers who spend a lot of time outdoors, but anyone can develop a Pterygium.
Are Pterygia dangerous?
Pterygia are not dangerous, although they can look unpleasant and cause some discomfort. The main problem with Pterygia is that as they grow onto the cornea they distort it, interfering with vision. If the Pterygium grows on to the central part of the cornea it can begin to block light from entering the eye. This can cause vision loss.
Although a Pterygium is not dangerous, it should be checked to make sure that it is not something more serious and that it is not progressing. If you have any area of tissue on or around the eyes that changes rapidly you should consult an optometrist or eye surgeon (ophthalmologist) immediately.
How can Pterygia be treated?
In cases where the Pterygium is not actively growing on to the cornea, protecting the eyes from ultraviolet light often will stabilise its growth. In many cases, provided it is not threatening vision and it remains stable, this may be all that is required. In cases where the Pterygium is actively growing on to the cornea and threatening to distort the vision, the only effective treatment is surgical removal. Fortunately this is relatively minor surgery that usually is performed under a local anaesthetic.
It is best to have surgery before the Pterygium progresses to the point where it interferes with vision. Your optometrist can assess the Pterygium and refer you to an eye surgeon if it requires removal.
How can Pterygia be prevented?
The best way to reduce your risk of developing a Pterygium is to protect your eyes from ultraviolet light. UV radiation can also cause Cataracts and other eye diseases, as well as skin cancers, so reducing exposure is a wise move. The best ways of doing this are to:
- Avoid the sun: in summer, three-quarters of outdoors UV exposure occurs between 10 am and 4pm. Staying out of the sun between those times will significantly reduce your UV exposure.
- Wear a hat: a broad-brimmed hat will not only protect your head from sunburn, but will reduce by at least half the amount of UV radiation reaching your eyes.
- Wear sunglasses: a good pair of sunglasses will reduce the amount of UV reaching your eyes and cut the amount of glare. Wrap-around sunglasses are best as they block UV radiation that can slip around the sides of conventional sunglasses.
